Scientists keep underestimating the coronavirus. In the beginning of the pandemic, they said mutated versions of the virus wouldn't be much of a problem—until the more-infectious Alpha caused a spike in cases last fall. Then Beta made young people sicker and Gamma reinfected those who'd already recovered from COVID-19. Still, by March, as the winter surge in the U.S. receded, some epidemiologists were cautiously optimistic that the rapid vaccine rollout would soon tame the variants and cause the pandemic to wind down.
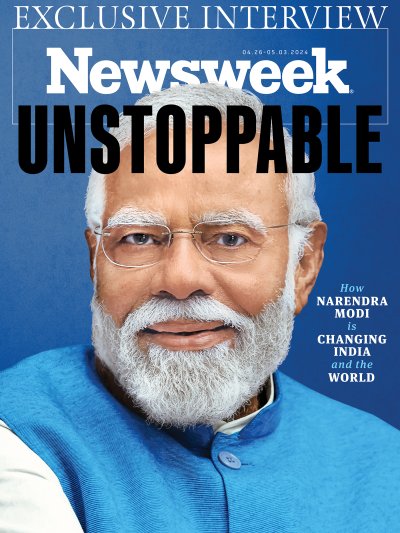
Delta has now shattered that optimism. This variant, first identified in India in December, spreads faster than any previous strain of SARS-CoV-2, as the COVID-19 virus is officially named. It is driving up infection rates in every state of the U.S., prompting the Centers for Disease Control and Prevention (CDC) to once again recommend universal mask-wearing.
The Delta outbreak is going to get much worse, warns Michael Osterholm, an epidemiologist who leads the Center for Infectious Disease Research and Policy at the University of Minnesota. "The number of intensive-care beds needed could be higher than any time we've seen," he says. He adds that his team's analysis shows that almost every single one of the 100 million unvaccinated Americans who hasn't had COVID-19 yet will likely get it in the coming months, short of taking the sort of strong isolation and masking precautions that seem unlikely in the vaccine-hesitant population.
The variant is so contagious that it's set to smash through every previous prediction of how soon the U.S. might reach herd immunity. "We've failed to shut this down as we have other pandemics," says Jonathan Eisen, a biologist at the University of California, Davis, who studies how pathogens evolve. "It may be around forevermore, leaving us continually trying to figure out what to do next."

Delta, like most of the other variants, blindsided us, worsening and extending the pandemic. When the damage from Delta starts to subside, what other variants will be lurking just behind it to pull us back down again? The World Health Organization is already keeping an eye on several: Eta, which is now in several countries; Kappa, which arose in India; Iota, which first popped up in New York City—and especially Lambda, which has torn through Peru and shows signs of having unusual success in infecting fully vaccinated people, according to one early study. It has already spread to Argentina, Chile, Ecuador as well as Texas and South Carolina.
It's too soon to say whether Lambda will turn out to be the next big, bad thing that COVID-19 unleashes on us. But it's a good time to wonder: Just how destructive can these variants get? Will future variants expand their attack from the lungs to the brain, the heart and other organs? Will they take a page from HIV and trick people into thinking they've recovered, only to make them sick later? Is there a Doomsday variant out there that shrugs off vaccines, spreads like wildfire and leaves more of its victims much sicker than anything we've yet seen?
The odds are not high that we will see such a triple threat, but experts can't rule it out. Delta has already shown how much worse things can get. Its extreme contagiousness, with room to run freely through the tens of millions of Americans who haven't been vaccinated and millions more who have no access to vaccines in developing countries, has good odds of turning into something even more troublesome. "The next variant," says Osterholm, "could be Delta on steroids."
Caught Off-Guard
It wasn't supposed to happen this way. Early in the pandemic, most experts closely studying COVID-19 mutations downplayed the notion that variants would cause such serious problems. "They don't seem to make much of a difference," said Richard Neher, an evolutionary biologist at Switzerland's University of Basel, in August last year. "We probably only need to worry about it on a timescale of about five years." Today he calls Delta and other COVID-19 variants "the pandemic within the pandemic."
Delta, more than any other variant, has reset scientists' understanding of how quickly a virus can evolve into devastating new forms. "All coronaviruses mutate, and we knew this one was mutating, too," says Sharone Green, a physician and infectious disease researcher at the University of Massachusetts Medical School. "But we didn't think the mutations would so strikingly affect transmissibility and possible evasion of immunity."
It may seem surprising that scientists were caught off-guard by the rapid emergence of a more dangerous variant. But unlike most other pathogens, Eisen notes SARS-CoV-2 was largely unknown when it emerged. In the absence of data, scientists assumed it would follow other viruses in being relatively slow to spin off much more contagious mutations. Even more important, he adds, scientists underestimated the sheer scale the pandemic would eventually achieve—a critical factor, because the more people a virus infects, the more opportunities it has to develop significant mutations. "Having billions of people infected presents a breeding ground for variants unlike anything we've ever seen with these sorts of viruses," he says.
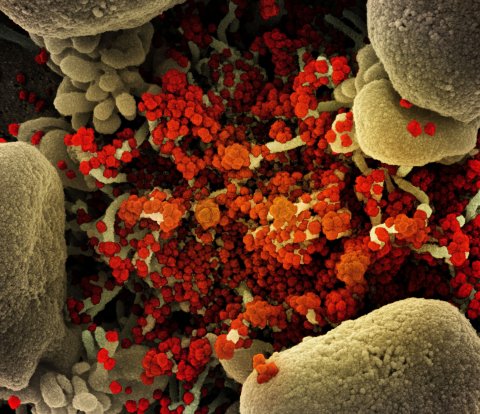
SARS-CoV-2 doesn't mutate particularly quickly, compared to many pathogens. Just as with most human and other cells, a mutation occurs in a virus when it replicates but fails to make a perfect copy of its genetic material. That imperfect copy is a mutant. The COVID-19 virus doesn't have a lot of genetic material to scramble compared to most organisms—about 15 genes, versus about 3,000 genes in an E. coli bacterium, a run-of-the-mill stomach bug, and about 20,000 in a human cell. What's more, COVID-19 has genetic checking mechanisms that make it reasonably adept at avoiding replication mistakes compared to most viruses.
But while COVID-19's mutation rate is on the low side—about one mutation for every 10 replications, or around a fifth of the flu's mutation rate and a tenth of HIV's—COVID-19 takes advantage of a grim numbers game. A single person infected with COVID-19 might carry 10 billion copies of the virus, enough to produce billions of mutated viruses every day. What happens to all those mutations? Almost always the answer is: nothing. The genetic scrambling is random, with the result that virtually all mutations either have no effect whatsoever on the virus, or else do something that makes the virus less effective or even renders it entirely non-functional.
But once in a while—perhaps every million trillion times—a random mutation confers some potentially dangerous new characteristic. What's more, much of what makes the virus dangerous has to do with a relatively small portion—the so-called spike proteins that protrude from its surface and enable the virus to latch onto and penetrate human cells. Most of the mutations we've seen so far represent tweaks to these spikes, which means it only takes a minimal change within any of the few viral genes that control the spikes to create a newly threatening mutation.
But even when a virus hits the jackpot with a mutation that sharpens its ability to wreak havoc, that doesn't mean a dangerous new variant has emerged. To become a significant variant, a mutated virus has to out-replicate the far more numerous copies of the virus that already predominate in the population, and to do that it needs features that give it big advantages.
What specific features will help the mutation become a better replicator and spreader in the population is determined by the environment. For example, in the case of a respiratory virus like COVID-19, the ability to travel longer distances in the air, and to latch more firmly onto cells in the nasal passage, would likely make a new strain a better contender to become a widely spreading variant.
"A virus' job is just to keep propagating," says Green. "Any mutation that helps the virus survive and spread will make it more successful as a variant."
All told, the chances that a virus in the population will produce a much more dangerous variant in the course of a year would normally be extremely low. But when billions of people are infected with billions of copies of a virus, all bets are off. Thanks to Delta's infectiousness, and the huge number of people whose refusal or inability to get vaccinated leaves them primed to become living COVID-19 mutation labs, the conditions are ripe to produce yet more, potentially more dangerous, variants in the coming months.

"It's going to be very difficult to stop it from happening with masks and social distancing at this point," says Preeti Malani, a physician and infectious disease researcher and chief health officer at the University of Michigan. "Vaccines are the key, and vaccine hesitancy is the obstacle."
The growing number of people with natural immunity, from having recovered from COVID-19, won't save the day either, says Eric Vail, director of molecular pathology at Cedars-Sinai Medical Center. "At best it's now a third of the U.S. population with natural immunity, and that may be an overestimation," he says. "It won't be enough to guarantee that Delta will be the last big variant."
Can It Beat the Vaccine?
The most likely way a new variant will plague us is the same way the U.K. variant did earlier this year, and Delta is now: by being more transmissible. At first glance, that seems a tall order, given that Delta is already one of the most transmissible viruses ever encountered, falling short only of the measles. Then again, notes Osterholm, scientists thought the original COVID-19 virus was a shockingly adept spreader, only to be surprised by how much more easily the U.K. variant spread, just to be caught off guard yet again with the rise of Delta, which is about five times more transmissible than the original.
There's no reason to assume Delta represents any sort of ceiling in infectiousness. "I wouldn't be incredibly surprised if something else came along that's even more transmissible," says Vail. Such a super-spreading virus might burn through the unvaccinated, non-previously infected population so fast that hospitals couldn't come close to coping.
Making that possibility more likely is the fact that sheer transmissibility, more than any other characteristic a virus might acquire through mutation, confers the greatest advantage on a variant when it comes to outcompeting other versions. "If a mutation comes up anywhere that's more transmissible, it will be selected out to propagate," says Green. That means a single ultra-transmissible mutation popping up anywhere in the world in a single infected person could be enough to unleash a fresh round of heightened global misery.

Might a new variant get around the vaccine? Delta appears to be able to infect the vaccinated more readily than previous variants, reducing the major vaccines' effectiveness at preventing infection from about 95 percent to around 90 percent. (A recent Israeli study claimed the Pfizer vaccine's effectiveness plunges to 39 percent, but experts caution that the finding is an outlier that may not hold up.)
Most of the COVID-19 vaccines work by getting human antibodies to target the spike proteins on the virus. But because mutations can slightly change the shape of the spike protein, they can potentially disguise it from some of those antibodies, thus weakening the vaccine's effectiveness. The different variants have different combinations of mutations in the spike protein, and while so far none of those combinations seem to do a great job of disguising the spike protein enough to get around the vaccine, some seem able to chip away at its effectiveness. Delta has three mutations that together seem especially good at keeping the spikes under the antibodies' radar, leading to the breakthrough infections.
Still, the vaccines remain highly effective in preventing Delta from causing severe illness leading to hospitalization or death, to judge by the fact that 99 percent of the patients struggling with COVID-19 in U.S. intensive-care units are unvaccinated.
COVID-19 may well continue to evolve into new, widely spreading variants, but there's reason to think that none of them are likely to routinely blow past the immune defenses conferred by vaccine, and even the lesser natural-immunity defenses. One reason, notes Vail, is that the vast majority of COVID-19 virus in circulation is in unvaccinated people who weren't previously infected, and mutations that can avoid immunity have no real advantage in that environment. An immune-evading variant would be more likely to thrive in a population of vaccinated or recovered people, where such a mutation would allow it to outcompete non-mutated viruses—but there just isn't enough virus circulating in that population to allow for rapid mutation.
That's how Delta emerged, notes Vail. "There were four variants that arose in India, and three of them had some ability to evade immunity," he says. "The fourth one was Delta, which didn't have as strong an evading mutation, and that's the one that spread."

Green points out a second reason being immune-evasive will be a huge challenge to COVID-19: The human immune system, once it's activated by vaccination or infection, is more resilient and effective than even most studies indicate. That's because studies tend to focus on how the virus fares against antibodies specifically developed by the body to fight the virus, as observed in test tubes. In real life, the body rolls out other weapons, including innate antibodies that target a broader array of pathogens, and T-cells that only kick in when an infection starts to take hold—both of which most lab studies can't easily measure. More thorough studies are underway, says Green, and the results should aid in the development of booster shots that will help block Delta and possible future variants.
The mechanics of mutation also work in our favor when it comes to dodging future variants that cause more severe illness. It's not that such mutations can't or won't spring up in the coming months. Rather, it's that causing the infected to be extremely ill takes them out of circulation, so they can't spread the more-sickening variant. That means the variant would be at a disadvantage to competing forms of the virus that leave most of the infected feeling well enough to walk around and transmit the infection.
A particularly dangerous scenario would be a variant that left people feeling well for a long time, and then lowered the boom later with severe illness. But few viruses—HIV being one exception—master that trick, and so far that doesn't seem to be a threat from COVID-19, either.
Eisen warns that such delayed-illness scenarios can't be ruled out, either. There are ways new variants could inflict worse damage without compromising their ability to spread. For example, a new variant might attack the brain, heart or other organs in more subtle, slower ways that leave victims walking around but that eventually take a large toll.
"We've already seen that different variants have differing abilities to enter some types of cells, and that might have an effect on the nervous system or lung function," says Eisen. "It's very concerning."
Malani notes that there's anecdotal evidence that more young people are getting severely ill with Delta than has been the case with previous variants. That uptick may just be due to higher numbers of young people getting infected, or it may indicate a troubling shift toward greater vulnerability among the younger. That wouldn't be a first: The 1918 flu pandemic preferentially killed younger adults.
It's not yet clear whether or not Delta is hitting the younger harder. "It's a mystery right now," Malani says. "Infected young people might walk around for days or even weeks even though they're feeling very poorly, so it's hard to judge." But even if Delta isn't targeting the younger, a spin-off variant might.

While increased infectiousness is the most likely path for a fierce post-Delta variant versus getting past vaccines or causing more severe illness, there's a catch: Such traits aren't mutually exclusive. Simply as a matter of chance, a mutation that confers increased transmissibility might also cause more damage to health or give the virus a better chance at slipping past the defenses conferred by a vaccine. Although these latter traits aren't likely to be selected on their own, they could ride the coattails of a transmissibility-boosting mutation. "There's nothing to stop them from happening at the same time," says Eisen.
Fortunately, there's a built-in impediment to what might otherwise be a potentially endless march toward ever-more-dangerous variants: The virus will at some point run out of ways to become nastier, thanks to the relatively simple structure of the spike protein, which can only be mutated in a few hundred different ways, most of which won't make the virus more harmful. "There are only so many changes that can be made to the spike protein without making it non-functional," says Vail. "I'd be cautious about saying that it can keep mutating indefinitely."
Another big break: Unlike the flu virus, SARS-CoV-2 doesn't have a structure that lends itself to mixing and matching genetic material between different variants. That "recombination" capability is what helps make the flu a moving target each year for vaccines.
Like the flu, COVID-19 is probably going to be with us for the foreseeable future. But a big pickup in vaccination rates would at least put the age of the most dangerous variants behind us. At that point, says Green, we can focus on occasional new vaccines or booster shots that make the virus a relatively tame threat.
"I don't think eradication is on the table," she says. "But I think we could come up with something that's better than what we have now for the flu."
On the other hand, notes Green, the flu kills as many as 60,000 people a year. If COVID-19 keeps mutating away from vaccine effectiveness and natural immunity, and a large portion of the population continues to neglect vaccinations, then we'll indeed end up permanently haunted by the virus.
In that case, we'd be lucky if COVID-19 "only" kills tens of thousands every year. Thanks to the ongoing threats of variants, we might be in for a lot worse.